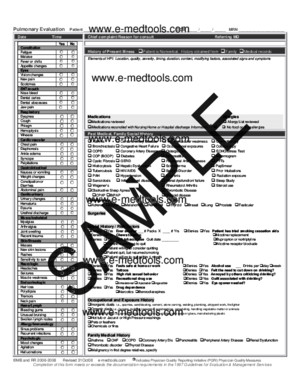
Pulmonary / Critical Care New Patient Evaluation
There is document - Pulmonary / Critical Care New Patient Evaluation available here for reading and downloading. Use the download button below or simple online reader.
The file extension - PDF and ranks to the Health & Medicine category.
Tags
Related
Comments
Log in to leave a message!
Description
The Pulmonary/Critical Care new patient evaluation MedicalTemplate is suitable for pulmonologists, critical care physicians, intensivists, hospitalists and other health care providers who evaluate patients with pulmonary or critical illnesses When completed, and in conjunction with a supporting level of medical decision making, this MedicalTemplate meets or exceeds the documentation requirements in the 1995 and 1997 Medicare Guidelines for E&M services for the highest level of service The pulmonary/critical care new patient evaluation MedicalTemplate contains prompters and space for all the required elements for a E&M encounter such as a H&P or Consult * History o Chief complaint o History of present illness o Past medical and surgical history o Social history + Risk factors for respiratory disease (occupational exposure, smoking, and others) o Family history o Review of systems + Yes/No checkboxes for clear and complete documentation * Examination o When completed, represents a comprehensive (highest) level physical exam as defined in 1997 Guidelines o Respiratory Single System Exam OR General Multisystem Exam o Checkboxes for pertinent negatives and common positive findings * Medical Decision Making o Full page for adequate space with complex patients o Easy Documentation with checkboxes + Review of labs, tests, imaging, old records + Coordination of care + Common diagnostic and therapeutic options o Assessment and plan
Transcripts
Pulmonary Evaluation Patient _________________________________________ DOB _____ / _____ / _____ MRN _____________________ ©MB and RR 2006-2008 Revised 31Oct08 e-medtoolscom Indicates Physician Quality Reporting Initiative (PQRI) Physician Quality Measures Completion of this form meets or exceeds the documentation requirements in the 1997 Guidelines for Evaluation Management Services Date Time Chief complaint/Reason for consult Referring MDHistory of Present Illness Patient is Nonverbal History obtained from Family Medical records Elements of HPI: Location, quality, severity, timing, duration, context, modifying factors, associated signs and symptoms Medications Allergies Medications reviewed Allergy List reviewed Medications reconciled with Nursing Home or Hospital discharge Information 46 No food or drug allergies Past Medical, Family Social History Yes NoConstitution Fatigue MalaiseFever or chills Appetite changes Eyes Vision changes New painScotomas ENT/mouth Nose bleedDental cariesDental abscessesJaw pain Respiratory DyspneaCoughPhlegmHemoptysisWheeze Cardiovascular Chest painDiaphoresisAnkle edemaSyncopePalpitations Gastrointestinal Nausea or vomitingWeight changesConstipation orDiarrheaAbdominal pain Genitourinary Urinary changesHematuriaDysuriaUrethral discharge Musculoskeletal MyalgiasArthralgiasJoint swellingRecent trauma Skin/Breasts MassesNew skin lesionsRashesSensitivity to sun Neurologic HeadachesSeizuresMuscle weakness Endocrinologic Hair lossPolydipsiaTremorsNeck pain Heme/Lymph Bleeding gumsUnusual bruisingSwollen lymph nodes Allergy/Immunology Sinus problemsRecurrent infections Psychologic Mood changesAgitationHallucinations Asthma Cerebral Artery Disease Neuromuscular weakness Chemotherapy Bronchiectasis Congestive Heart Failure Occupational exposures Colonoscopy COPD Coronary Artery Disease Osteoporosis ECHO/Stress Test COP (BOOP) Diabetes Pancreatitis Mammogram Cystic Fibrosis GERD Peripheral Artery Disease PFTs Histiocytosis Hepatic Dysfunction Scleroderma PapSmear Tuberculosis HIV/AIDS Seizure Disorder Prior Intubations PAH Hypertension Sjogren’s Radiation exposure Sarcoidosis Inflam bowel disease Renal dysfunction/ failure Sleep Study Wegener’s Malignancy Rheumatoid Arthritis Steroid use Obstructive Sleep Apnea Thrombotic Disease CPAP BiPAP Thyroid disease Malignancy Adrenal Colon Melanoma Renal cell Thyroid Breast Lung Prostate Testicular SurgeriesSocial History / Risk factors Denies Yes Ever smoker ___ # Packs X ____ # Yrs Denies Yes Patient has tried smoking cessation aids Denies Yes Chews tobacco Nicotine replacement Denies Yes Quit tobacco use Quit date _________ Buproprion or nortriptyline Patient is unwilling to quit Nicotine receptor blockade Patient willing to consider quitting Patient quit, but resumed smoking Patient willing to quit within 1 month Denies Yes Feels safe at home or work Denies Yes Alcohol use ___ Drinks per day week Denies Yes Tattoos Denies Yes Felt the need to cut down on drinking? Denies Yes High risk sexual behavior Denies Yes Annoyed by others criticizing drinking? Denies Yes Recreational drug use Denies Yes Guilt associated with drinking? Inhalational Injectable Ingestible Denies Yes Eye opener needed? Denies Yes Drug dependence Narcotics Benzodiazepines Occupational and Exposure History Inorganic dusts ie, quarries, sandblasting, cement, stone carving, welding, plumbing, shipyard work, firefighter Organic dusts ie, farming, building inspection, woodworking, remodeling, handling vegetable matter or animals Noxious fumes ie, spray painting, autobody work, working with dyes or glues, manufacturing plastic Hot tub or Jacuzzi or High Pressure washings Pets or feathers Chemicals or fires Family Medical History Asthma CHF COPD Coronary Artery Dis Pancreatitis Peripheral Artery Disease Renal Dysfunction Thrombotic disorder Thyroid Disease Malignancy in first degree relatives, specify Reset Reset Reset Reset Reset Reset Reset Reset Reset Reset Reset Reset Reset Reset Pulmonary Evaluation Patient _________________________________________ DOB _____ / _____ / _____ MRN _____________________ ©MB and RR 2006-2008 Revised 31Oct08 e-medtoolscom Indicates Physician Quality Reporting Initiative (PQRI) Physician Quality Measures Completion of this form meets or exceeds the documentation requirements in the 1997 Guidelines for Evaluation Management Services Exam To qualify as a comprehensive exam: General Multisystem requires performing ALL of ≥ 9 organ systems, AND ≥ 2 elements documented in each organ systemRespiratory Single Organ System Exam requires documentation of ALL highlighted organ system elements, AND ≥ 1 element in every other organ system is expected Ventilator, IV Medications Labs VentilatorMode AC SIMV PC PRVC Other ____________ Rate __________ Tidal Vol __________ PEEP __________ PS __________ FiO2 __________ PO2/FiO2 __________ Plateau _________ _ NonInvasive Ventilator CPAP BiPAP IV Medications Pressors Dose Rate ____________________________ ____________________________ Antihypertensives ____________________________ Diuretics ____________________________ Antibiotics ____________________________ ____________________________ Sedation ____________________________ Narcotics ____________________________ Heparin ____________________________ Insulin ____________________________ Antiarrhythmics ____________________________ Steroids ____________________________ Paralytic ____________________________ Thrombolytic ____________________________ TPN Labs \____/ / ____ / ____ / ____ / Constitutional ( ≥ 3 vitals) Body habitus and Grooming required of General Multisystem but not Organ System Exam Height ___________ in cm Weight ___________ lb kg Temperature __________ Pulse Rate __________ AND Rhythm Regular Irregular Blood Pressure sitting __________ / __________ OR standing __________ / __________ Blood Pressure lying __________ / __________ Respiratory Rate __________ Optional Sats _____ % Cardiac Output _____ SVR _____ Body habitus wnl Cachectic Obese Grooming wnl Unkempt ENT Nasal mucosa, septum, and turbinates wnl Dentition and gums wnl Dental caries Gingivitis Oropharynx wnl Oropharyngeal edema or erythema Oral ulcers Oral PetechiaeMallampati I II III IV Neck Neck wnl Erythema or scarring consistent with Recent Old radiation dermatitis Thyroid wnl Thyromegaly Thyroid nodules palpable Neck mass ___________________________ Jugular Veins wnl JVD present a, v or cannon a waves present Resp Chest is free of defects, expands normally and symmetrically Erythema consistent with radiation dermatitis Scarring consistent with old, healed radiation dermatitis Respiratory effort is wnl Accessory respiratory muscle use Intercostal retractions Paradoxic diaphragmatic movements Chest percussion wnl Dullness to percussion Lt Rt Hyperresonance Lt Rt Tactile exam wnl Tactile fremitus Increased Decreased _____________________________________ Clear to auscultation Bronchial breath sounds Egophony (E to A) Rales Rhonchi Wheezes Rub present ________________________ CV Clear S1 S2 No murmur, rub or gallop Gallop Rub Murmur present Systolic Diastolic Grade I II III IV V VI Peripheral pulses palpable No peripheral edema Peripheral pulses Absent Weak GI Abdominal exam wnl Mass present LUQ RUQ LLQ RLQ ____________________ Pulsatile Liver and spleen palpation wnl Unable to palpate Liver Spleen Enlarged Liver Spleen Lymph ( ≥ 2 areas must be examined) Lymph node exam wnl Areas examined Neck Axilla Groin Other ___________________ Lymphadenopathy noted in Neck Axilla Groin Other ___________________ Musc Muscle tone within normal limits, and no atrophy notedTone is Increased Decreased Atrophy present Gait and station wnl Ataxia Wide based gait Shuffle Patient leaning Rt Lt Front Back Extrem Exam wnl Clubbing Cyanosis Petechiae Synovitis Rt Lt ________________________ Skin No rashes, ecchymoses, nodules, ulcers Periungual telangiectasias Splinter hemorrhages Neuro Oriented 58(Pts with Community Acquired Bacterial Pneumonia) NOT oriented to Person Time Place Affect is within normal limits OR Patient appears Agitated Anxious Depressed Glasgow Coma Score E _____ V _____ M _____ APACHE II Score __________ Pulmonary Evaluation Patient _________________________________________ DOB _____ / _____ / _____ MRN _____________________ ©MB and RR 2006-2008 Revised 31Oct08 e-medtoolscom Indicates Physician Quality Reporting Initiative (PQRI) Physician Quality Measures Completion of this form meets or exceeds the documentation requirements in the 1997 Guidelines for Evaluation Management Services Data Reviewed Impression ER Notes Old medical records Labs Radiology data ECHO ECG Stress Test Pulmonary Function Test Nursing Notes/Vitals log Care Coordinated with Patient HCPOA / Surrogate PCP Consultant Case Management or Social Worker Pharmacy Nursing Physical Therapist Occupational Therapist Speech Therapist Recommended Actions Aggressive pulmonary toilet DVT prophylaxis Stress ulcer prophylaxis Daily sedation vacation andneurologic assessment Head of bed elevated > 30 Degreesat all times Intense glycemic control Insulin infusion Central line change or removal (send tip for culture) Physical therapy Enteral/Parenteral feeds Smoking cessation aids Pneumonia vaccine prior to discharge Influenza vaccine prior to discharge Recommended Diagnostics PPD Testing 12-lead EKG Echocardiogram Sputum culture Bacterial Fungal AFB Blood culture Urine culture CSF culture CBC with differential PT, PTT, INR BMP (with calcium) HIV Hepatitis panel Code Status Patient is a FULL CODE DO NOT ATTEMPT RESUSCITATION Patient has completed advanced health care directives 47 HCPOA is _______________________________________ Signature ________________________________________ cc __________________________________
Recommended