Multimillion-Dollar Healthcare Insurance Fraud Lawsuit against Johnson Johnson Filed in CA
There is document - Multimillion-Dollar Healthcare Insurance Fraud Lawsuit against Johnson Johnson Filed in CA available here for reading and downloading. Use the download button below or simple online reader.
The file extension - PDF and ranks to the Documents category.
Tags
Related
Comments
Log in to leave a message!
Description
Download Multimillion-Dollar Healthcare Insurance Fraud Lawsuit against Johnson Johnson Filed in CA
Transcripts
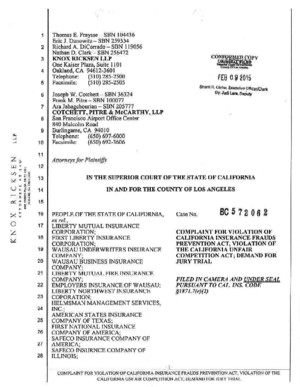
PRESS RELEASE FOR IMMEDIATE RELEASE For more information, contact: June 24, 2015 Charles F Kester, Esq Delaney Kester LLP Tel: 818-974-8627 charlesdelaneykestercom Ilyas J Rona, Esq Delaney Kester LLP Tel: 617-671-9510 ilyasdelaneykestercom Multimillion-Dollar Insurance Fraud Lawsuit against Johnson Johnson Announced in California CALABASAS, CA— JUNE 24, 2015 —Delaney Kester LLP announces that it is bringing a multimillion-dollar insurance fraud lawsuit against Johnson Johnson and its subsidiary Acclarent, Inc in Los Angeles Superior Court The lawsuit seeks damages in connection with the MicroFlow Spacer, a medical device marketed by Johnson Johnson and Acclarent to treat sinusitis The whistleblower complaint – which is brought under California Insurance Code § 18717 by a former employee of Johnson Johnson and Acclarent – alleges that the MicroFlow Spacer was only on the market because of false statements made to the FDA As a result, all costs associated with the device were ill-gotten and the Johnson Johnson and Acclarent caused health insurers to pay claims that would not have been paid otherwise Johnson Johnson claims to be the world’s largest medical device manufacturer In January 2010, Johnson Johnson’s subsidiary Ethicon purchased Menlo Park, CA startup Acclarent for 785 million Johnson Johnson continued to sell MicroFlow Spacers until 2013 Two months ago, the US Department of Justice announced an indictment against Acclarent’s former CEO William Facteau and its Vice President of Sales Patrick Fabian for various counts of conspiracy, wire fraud, and introducing adulterated or misbranded medical devices into interstate commerce The indictment alleges that Acclarent’s former executives fraudulently increased company revenues by illegally marketing the MicroFlow Spacer for uses not cleared or approved by the FDA This increased revenue came at the expense of public and private payors, including health insurance companies Delaney Kester LLP seeks to obtain compensation for private health 2 insurers and, by extension, the policyholders whose premiums increase anytime fraud goes undetected in the healthcare system California Insurance Code § 18717 allows “interested persons” to file complaints targeting fraudulent billing to private insurers The statute is modeled after the federal False Claims Act (the “FCA”); but unlike the FCA, which seeks to recover federal funds wrongly paid by programs such as Medicare and Medicaid, Section 18717 provides a remedy when private insurers are defrauded As the California Insurance Code observes, health insurance fraud is a “particular problem” for all Americans Although there are no precise figures, it is estimated that healthcare fraud adds billions of dollars every year in unnecessary healthcare costs and higher premiums across the country The complaint is brought by attorneys of Delaney Kester LLP , including Charles F Kester of Calabasas, California, and Royston H Delaney and Ilyas J Rona of Boston, Massachusetts; and by attorneys of Kellogg, Huber, Hansen, Todd, Evans Figel, PLLC , including Silvija A Strikis and Joseph S Hall of Washington, DC The media contacts listed at the top are available for interviews —End—



![[TAX] Commissioner of Internal Revenue vs SC Johnson and Son Inc, And CA](imgdoc/93201.jpg)